Spinal cord injuries occur in the United States at a rate of approximately 12,000 injuries each year. The largest proportion (36.5 percent) are a result of car accidents. The next most common causes occur as a result of falls, followed by acts of violence (primarily gunshot wounds), and sporting accidents.
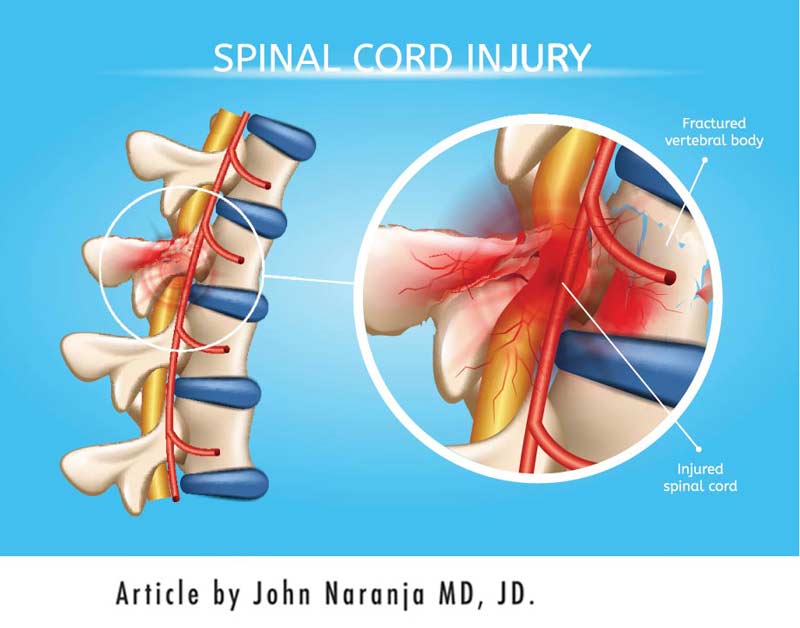
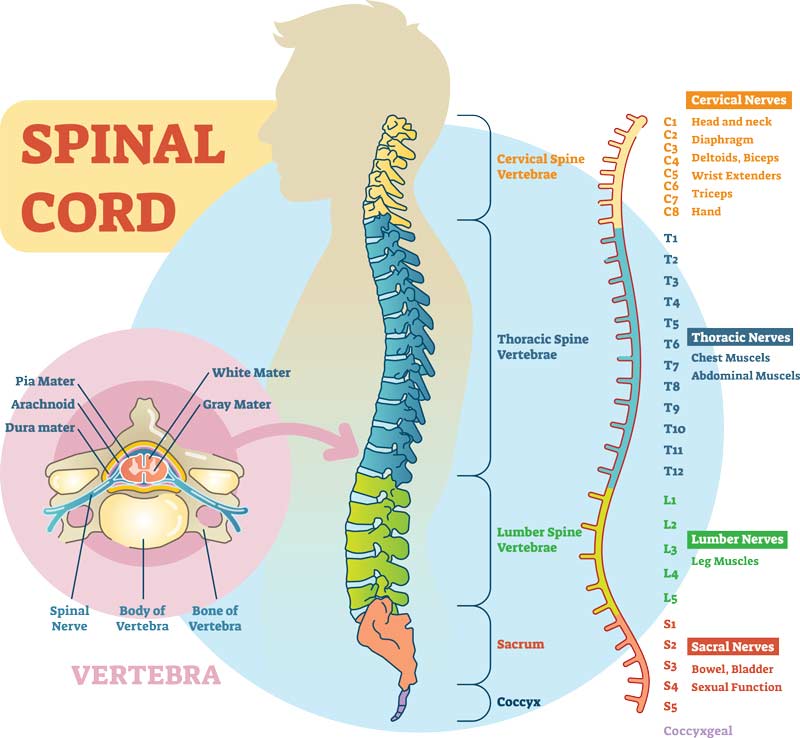
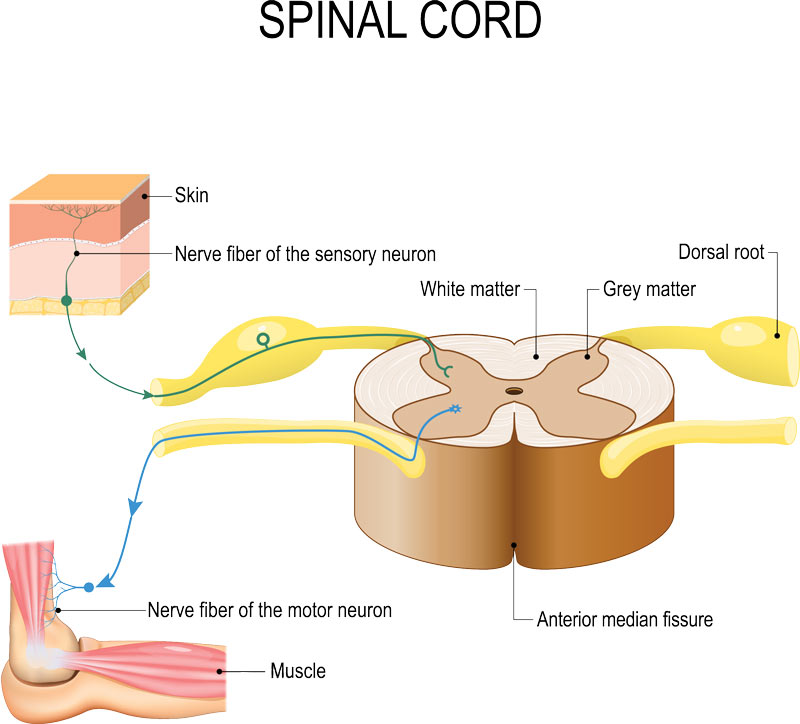
Injuries to the spinal cord can be catastrophic because of the central role the spinal cord has in governing our interactions with the environment. In particular, the spinal cord possesses nerves that communicate with our brain to inform about external stimuli. It also contains nerves that control the way we move and respond to both internal and external influences. Nerves can be thought of as the electrical wires of our body that transmit information and commands to and from the brain.
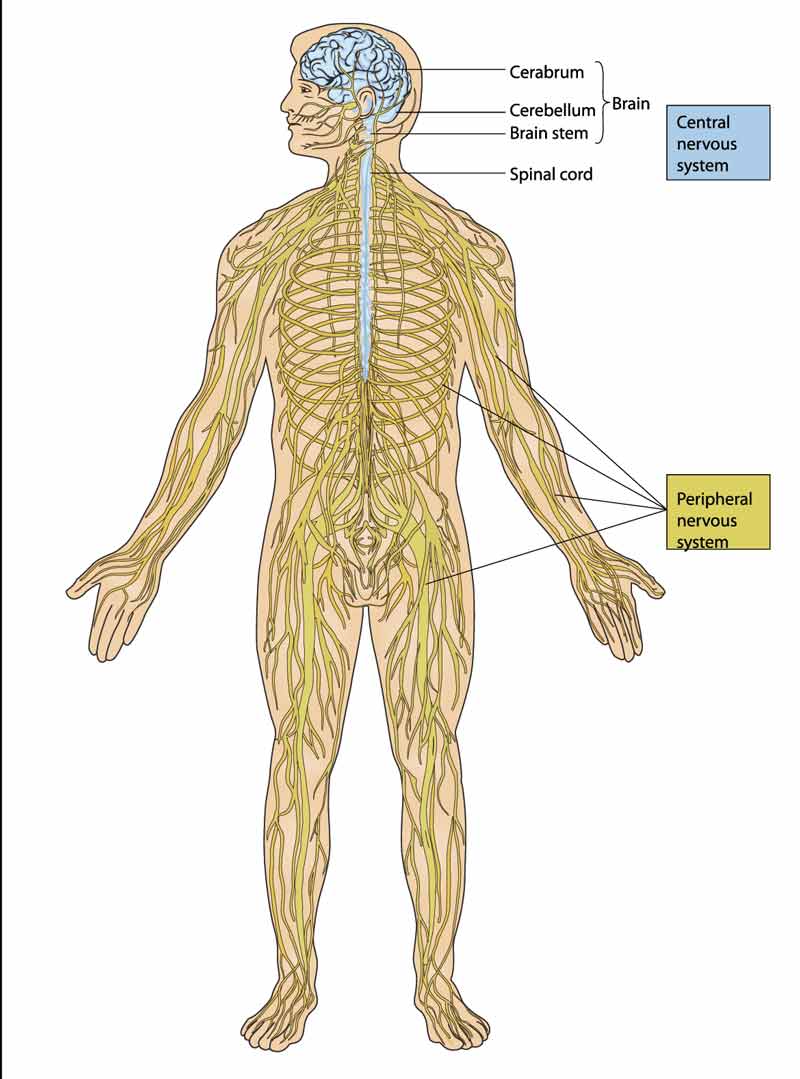
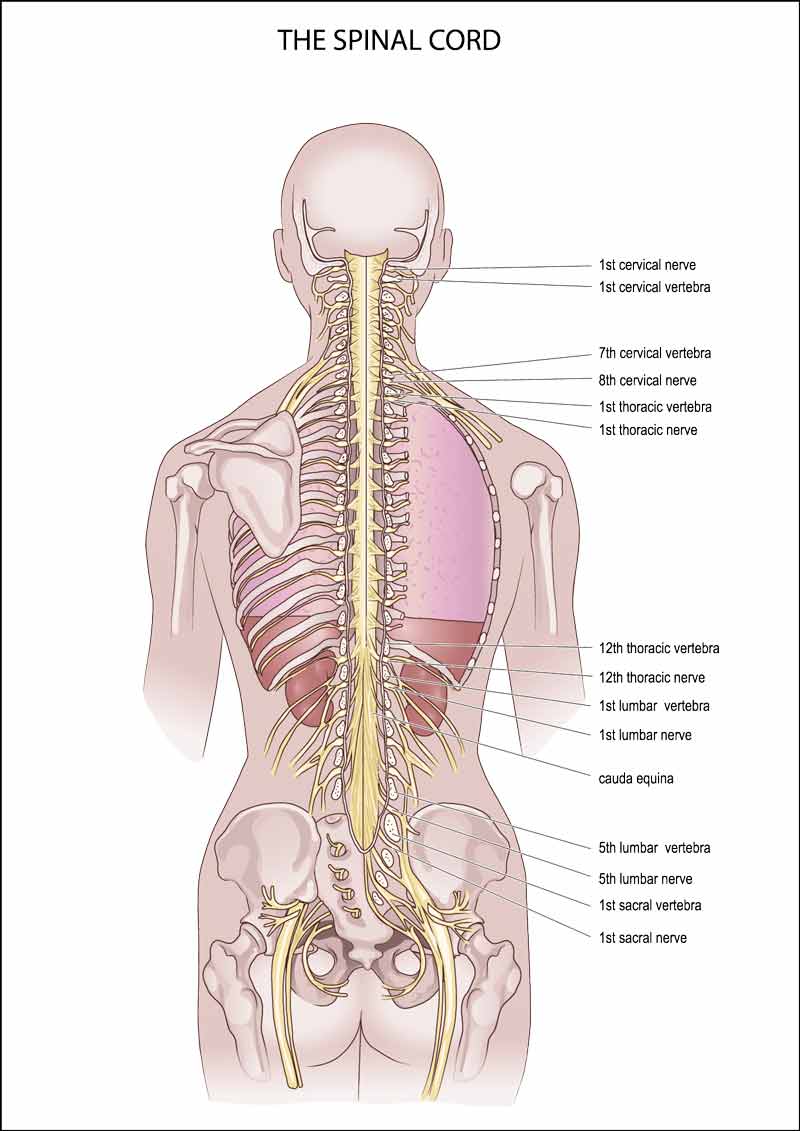
The nerves from the spinal cord are mapped to specific areas of the body. Accordingly, the nerves of the spinal cord can be categorized by their location. Specifically, the parts of the spine and spinal cord are classified as cervical, thoracic, lumbar, sacral, and coccygeal.
Those nerves closest to the brain tend to control the upper part of the body and extremities, while those nerves traveling further away from the brain control the lower part of the body and extremities in sequence.
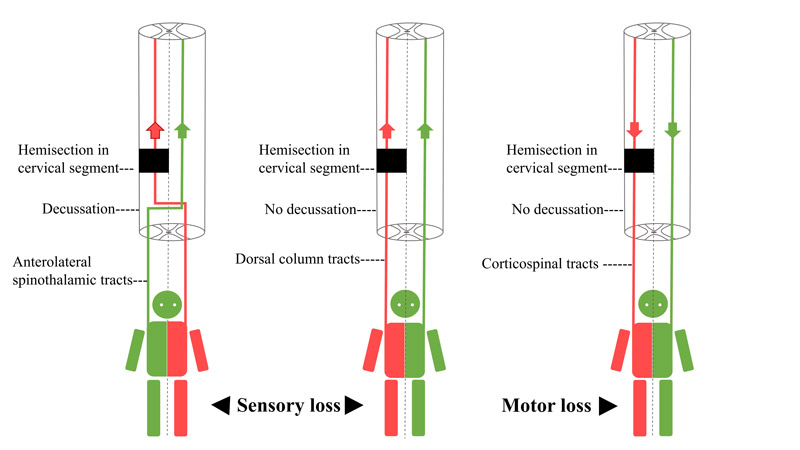
The spinal cord anatomy is also divided at each level by the location of the nerves in the spinal cord with respect to the front and back of the body. The anterior nerves (or front part of the cord) are generally responsible for movement and the posterior nerves (or back part of the cord) are generally responsible for sensation. The nerves are also categorized by the side of the body where the nerves are directed (i.e. right or left).
The effect of injuries to the spinal cord in large part depends on the level, location, and side at which the cord is traumatized. The diagnosis of the level is facilitated by testing different parts of the body for any deficit in sensation or movement.
Medical providers use standard techniques to measure sensation and movement. Sensation is scored on a three-point scale by comparing the sensation to a patients’ cheek as a normal frame of reference. The scale can be summarized as follows:
- 0 = absent
- 1= altered (impaired or partial appreciation, including hyperesthesia or an increase in sensation)
- 2 = normal or intact (similar as on the cheek)

Muscle strength and movement is graded on a six-point scale: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3232636/
- 0 = total paralysis or no movement
- 1 = palpable or visible contraction or twitching of the muscle
- 2 = active movement, full range of motion (ROM) with gravity eliminated.
- 3 = active movement, full ROM against gravity.
- 4 = active movement, full ROM against gravity, and moderate resistance in a muscle specific position.
- 5 = (normal) active movement, full ROM against gravity, and full resistance in a muscle specific position expected from an otherwise unimpaired person.
- 5* = (normal) active movement, full ROM against gravity, and sufficient resistance to be considered normal if identified inhibiting factors (i.e. pain, disuse) were not present.
- NT= not testable (i.e. due to immobilization, severe pain such that the patient cannot be graded, amputation of a limb, or contracture of >50% of the range of motion).

Testing is usually performed over time to compare responses. Testing is also more meaningful after a week to 10 days from the time of the traumatic event. This is because swelling in the spinal cord can confuse the results of an exam and needs time to subside. The early time when there is neurologic deficit related to swelling from a spinal cord injury is called spinal shock.
Types of Complete Spinal Cord Injury
Once spinal shock is over, and there remains complete loss of motor and/or sensory function, a number of terms require understanding.
Tetraplegia, also called quadriplegia refers to complete loss of motor and/or sensory function in the cervical region. As the term tetra- and quad- imply, this type of injury results in impairment of function in all four extremities. More precisely, this typically includes the arms, trunk, pelvic organs, and legs.
Paraplegia refers to complete loss of motor and/or sensory function in the non-cervical portions of the spinal cord. This means the thoracic, lumbar, or sacral part of the spinal cord has been injured. Accordingly, paraplegia is distinguished from tetraplegia because arm functioning is typically maintained.
Tetraparesis and paraparesis refer to partial loss of motor and/or sensory function. Tetra- again refers to impairment in the cervical region, and para- refers to impairment in non-cervical regions.
Use of these terms has been discouraged, however, as they describe incomplete lesions insufficently. Instead, the American Spinal Injury Association Impairment Scale (AIS) has been favored as a more precise approach to the description of the severity (i.e. completeness) of spinal cord injuries. A complete versus incomplete injury is dependent on the presence and/or extent of “sacral sparing” or function of those nerve in the buttock region.
- A = Complete Spinal Cord Injury. No sensory or motor function is preserved in the sacral segments S4-S5.
This means that for the area in the sacrum (just above the tailbone), there is no sensation in the buttocks region and no control of holding one’s bowels.
- B = Sensory incomplete. Sensory but not motor function is preserved below the neurological level and includes the sacral segments S4-S5, AND no motor function is preserved more than three levels below the motor level on either side of the body.
This means that for the area in the sacrum, there is sensation in the area of the buttocks.
- C = Motor incomplete. Motor function is preserved below the neurological level, and more than half of key muscle functions below the single neurological level of injury have a muscle grade less than 3 (Grades 0–2).
This means that there is still some function, though very weak, of bowel motor control.
- D = Motor incomplete. Motor function is preserved below the neurological level, and at least half (half or more) of key muscle functions below the neurologic level of injury have a muscle grade >3.
This means that the function of bowel motor control is present, though weak
- E = Normal. If sensation and motor function as tested are graded as normal in all segments, and the patient had prior deficits, then the AIS grade is E. Someone without a spinal cord injury does not receive an AIS grade.
An incomplete spinal cord injury indicates that there is a chance for at least some rehabilitation and/or recovery.

Incomplete spinal cord injuries have also been described as clinical syndromes and it is useful to understand these terms.
Central cord syndrome
Central cord syndrome is the most common of the clinical syndromes with incomplete spinal cord injury. It is often seen in patients with cervical arthritis who sustain a hyperextension injury from a fall. Symptoms are characterized by greater weakness in the upper limbs than in the lower limbs.
Brown-Sequard syndrome
Brown-Sequard syndrome represents a spinal cord injury that is sustained to either the left or right side of the cord. Historically, this occurred from a knife wound to one side of the spinal cord. From a muscle strength standpoint, there is loss or weakness of the body on the side of the injury. Sensation, however, follows a different pattern. Pain and temperature is lost on the opposite side of the injury and vibration and proprioception (the ability to be aware of one’s body position in space) is lost on the same side as the injury.
Anterior cord syndrome
The anterior cord syndrome is a relatively rare incomplete spinal cord syndrome. It has been related to a decreased or absent blood supply to the anterior part of the spinal cord. The clinical symptoms include a loss of strength, pain sensation, and temperature sensation at and below the injury level with preservation of light touch and proprioception.
Cauda equina syndrome
The lowest part of the spinal cord stops at approximately the lumbar L1-2 level. The remaining nerves beyond this area are called the cauda equina. Cauda Equina syndrome involves the nerve roots of the cauda equina and will produce paralysis of the muscles of the lower limbs and loss of bowel and bladder control. Sensation is also lost below the level of the lesion.
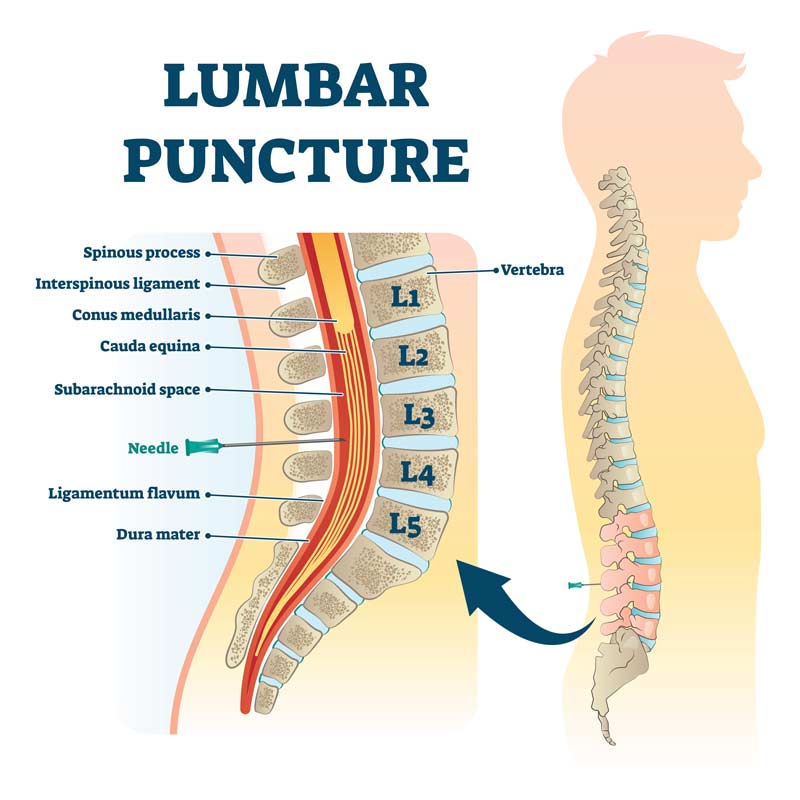
Conus medullaris syndrome
Just above the cauda equina at L1-2 is the conus medullaris. Conus Medullaris Syndrome may clinically be similar to the Cauda Equina Syndrome, but the injury is further up the cord above the L1 and L2 area.
Conclusion
Spinal cord injuries represent a wide spectrum of injuries that can be distinguished based on symptoms and understanding the anatomy of the spinal cord.
Dr. John, Esq. is both an attorney and a physician. Before obtaining his law degree, Dr. John Naranja practiced for approximately 12 years as an orthopedic surgeon.